Central Line (Central Venous Access Device)
You need a central line as part of your treatment. It’s also called a central venous access device (CVAD) or central venous catheter (CVC). A small, soft tube called a catheter is put in a vein that leads to your heart. When you no longer need the central line, it will be taken out. Your skin will then heal. This sheet describes types of central lines. It also explains how the central line is placed in your body.
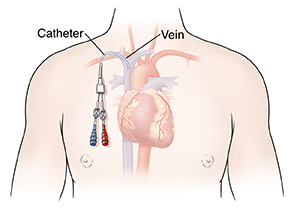 |
| The catheter may have more than 1 channel. This means that different fluids or medicines can be given at the same time. |
What a central line does
A central line is often used instead of a standard IV (intravenous) line when you need treatment for longer than a week or so. The line can deliver medicine, fluids, or nutrition right into your bloodstream. It can also be used to measure blood flow (hemodynamic monitoring), to draw blood, or for other reasons. Ask your healthcare provider why you need the central line and which type you’ll get.
Types of central lines
The central line will be placed into one of the veins as described below. Which vein is used depends on your needs and overall health. The catheter is threaded through the vein. It is passed along until the tip sits in the large vein near the heart (vena cava). Types of central lines include:
-
Peripherally inserted central catheter (PICC). This line is placed in a large vein in the upper arm, or near the bend of the elbow.
-
Subclavian line. This line is placed into the vein that runs behind the collarbone.
-
Internal jugular line. This line is placed into a large vein in the neck.
-
Femoral line. This line is placed in a large vein in the groin.
Placing the central line
The central line is placed in your body during a short procedure. This may be done in your hospital room, the emergency department, or an operating room. Your healthcare team can tell you what to expect. During central line placement:
-
You’re fully covered with a large sterile sheet. Only the spot where the line will be placed is exposed. The skin is cleaned with antiseptic solution. These steps lower the risk for infection.
-
Medicine (local anesthetic) is injected near the vein. This numbs the skin so you don’t feel pain during the procedure.
-
After the pain medicine starts to work, the catheter is gently passed into the vein. It’s moved forward until the tip of the catheter is in the vena cava, close to the heart. This is usually done with the help of an ultrasound machine. The ultrasound machine helps see below the skin. It helps the provider guide the catheter into the vein without hurting other tissues or organs.
-
The other end of the catheter extends a few inches out from your skin. It may be loosely attached to the skin with stitches to hold it in place.
-
The healthcare provider flushes the catheter with saline solution to clear it. The solution may include heparin. This prevents blood clots.
-
An X-ray or other imaging test is done. This allows the provider to confirm the catheter’s position and check for problems.
Risks and possible complications
As with any procedure, having a central line placed has certain risks. These include:
-
Infection
-
Bleeding problems
-
An irregular heartbeat
-
Injury to the vein or to lymph ducts near the vein
-
Inflammation of the vein (phlebitis)
-
Air bubble in the blood (air embolism). An air embolism can travel through the blood vessels and block blood flow to the heart, lungs, brain, or other organs.
-
Blood clot (thrombus) that can block the flow of blood. A blood clot can also travel through the blood vessels. It can block blood flow to the heart, lungs (pulmonary embolism), brain, or other organs.
-
Collapsed lung (pneumothorax) or blood buildup between the lungs and the chest wall (hemothorax)
-
Nerve injury
-
Accidental insertion into an artery instead of a vein
-
Catheter not positioned correctly
If you have any problems with your central line, talk with your healthcare provider.